Previously was necessary to transplant the entire cornea when keratoplasty was performed, however currently is possible to transplant only the area of the affected cornea. Indeed, the advent of femtosecond laser has allowed that keratoplasty be more precise and safety intervention. Specifically, femtosecond laser in keratoplasty surgery is used to create the donor corneal button, as for eliminate the cornea where will be grafted the corneal button. Nevertheless, the microkeratome can be used to prepare the corneal graft if not is available femtosecond laser technology.
Different causes can produce the need for a corneal transplant. The most common cause of keratoplasty in corneal ectasia is keratoconus. Precisely, Anterior Lamellar Keratoplasty (ALK) in patients with keratoconus is conducted when crosslinking, rigid contact lenses or intraestromal corneal rings do not reduce the progression of the pathology. Besides of corneal ectasia others causes require corneal transplant, like endothelial cell loss, or infections among others… Depending of the corneal area to be transplanted different variants of keratoplasty has been developed, and it is necessary to known properly.
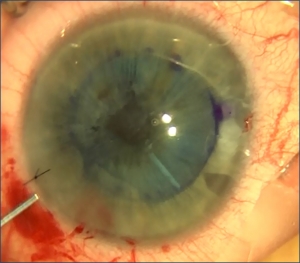
Left: Intra-Operative Descemet Membrane Endothelial Keratoplasty (DMEK). Center: Post-Operative DMEK. Right: Deep Lamellar Endothelial Keratoplasty (DLEK).
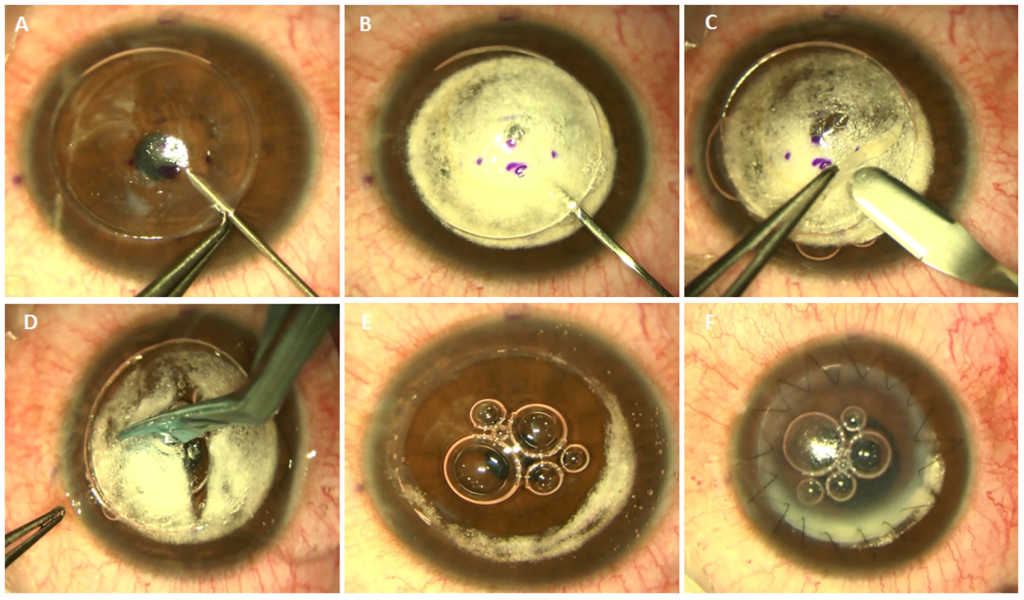
Deep Anterior Lamellar Keratoplasty (DALK) “step by step”.
In the “Online Course Clinical Methodology in Refractive Cataract and Corneal Surgery” provide adequate training on the surgical procedures according to the different variants of keratoplasty. Precisely, the international tutors of the online course recognized with 25 ECTS credits by University Miguel Hernandez, are experts surgeons in keratoplasty techniques. Moreover, the scientific recognition of the international tutors is manifest. Specifically, the professor of the course Dr Mahmoud Ismail participated the last February 11 in the DALK workshop Menia University. Tutor international of the course, Dr Mahmoud Ismail will be moderator the next March 16-18 of the symposium “towards suturless keratoplasty” in the Egyptian Society of Ophthalmology. Due to the presence of the experimented international tutors in keratoplasty, through of our training program, ophthalmologists will acquire a high knowledge of the assessment by means of clinical devices, as possible complications pre- and post-surgical.
What devices are used for clinical assessment in patients undergo keratoplasty?
Scheimpflug devices corneal topographers provide useful information to evaluate topographic changes and corneal profile in patients undergo keratoplasty. Specifically, posterior corneal surface aberrations, astigmatism and dioptric power are highly important to evaluate after performing keratoplasty. Moreover, the corneal topographers that analyze the corneal densitometry, are devices very useful in post-keratoplasties. In addition to corneal topographers that analyzed both corneal surfaces, among the main clinical applications of Anterior Segment Optical Coherence Tomography (AS-OCT) keratoplasty highlights. The tomographical sections of the AS-OCT and the corneal topographers that analyzed both corneal surfaces allow assess the location of the corneal graft, as likewise analyze corneal thickness after keratoplasty. Both devices allow display the demarcation line between the patient’s cornea and corneal graft.
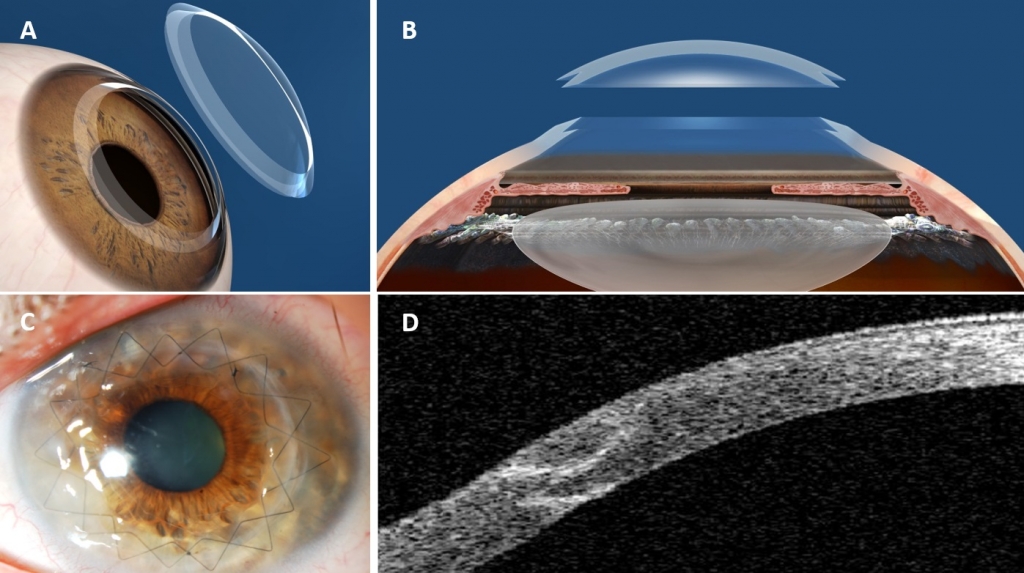
Scheme of a femtosecond laser assisted penetrating keratoplasy.
How are the options to improve vision after keratoplasty?
Keratoplasty increases irregular astigmatism and Higher-Order Aberrations (HOA). It has been shown that thicker grafts precisely produce greater increase in HOA than fine grafts. In order to improve the visual quality and reduce corneal complications, Photorefractive Keratectomy (PRK) is recommended after Penetrating Keratoplasty (PK) instead of Laser assisted in Situ Keratomileusis (LASIK), although it is necessary removed the sutures previously.
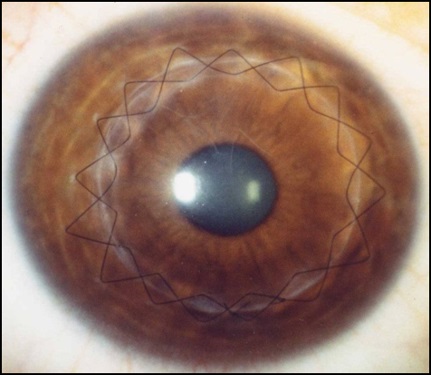
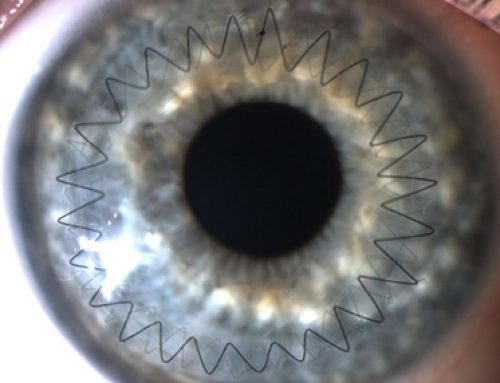
Post-operative picture of a Penetrating Keratoplasty for advanced keratoconus.
Another options for improve visual quality after keratoplasty are Arcuate Keratotomy (AK), corneal rings, and Intraocular Lenses (IOLs). Astigmatic incisions through of femtosecond laser are effective and safe for the correction of astigmatism after keratoplasty. Arcuate keratectomy precisely was developed for the correction of astigmatism in patients undergoes keratoplasty, but later due to the good outcomes has become popular. Sometimes it is possible to implant intrastromal corneal rings in patients undergo keratoplasty to regularize the corneal surface. Phakic IOLs are another option to improve optical quality after keratoplasty, in order to correct the astigmatism and high myopia. After implantation of Phakic IOLs, endothelial microscopy, AS-OCT, as corneal topographers that analyzed both corneal surfaces are devices very useful for the evaluation of the endothelial cell count, and for the analysis of the safety distance between the IOL iris fixation and corneal endothelium. If this distance is reduced it could decrease the number of endothelial cells, and endothelial keratoplasty would be required. In addition of phakic IOLs iris fixation, Posterior Chamber Phakic IOLs, or even pseudophakic IOLs are another options in patients undergo keratoplasty. Precisely, in one study published by Hjortdal in collaboration with others authors determined that aspherical IOLs may be implanted in patients undergoing Descemet’s Stripping Automated Endothelial Keratoplasty (DSAEK) because they don’t proved variations in spherical aberration. All the options for improve the optical quality and correct the refractive errors in patients undergo keratoplasty, will be properly explained in the “Online Course Clinical Methodology in Refractive Cataract and Corneal Surgery”.
Bibliographic references
Clemmensen K, Ivarsen A, Hjortdal J. Changes in Corneal Power After Descemet Stripping Automated Endothelial Keratoplasty. J Refract Surg. 2015 Dec 1;31(12):807-12.
Jorge L. Alió, Dimitri T. Azar. Management of complications in refractive Surgery. 2008 Springer-Verlag Berlin Heidelberg.