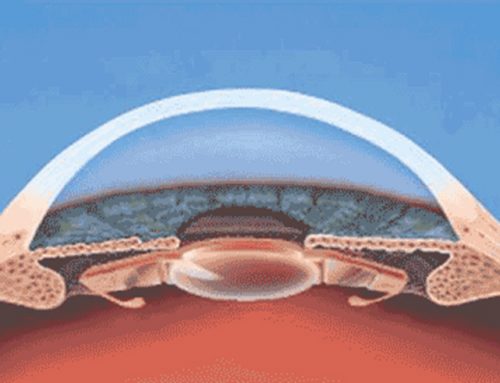
Presbyopia is a natural condition that induces difficulty to read in near distances in patients with age over 40 years approximately. The gradual loss of accommodative capacity to focus near objects in presbyopic patients is due to variations in the crystalline lens, ciliary muscle as in zonular fibres. Precisely, presbyopia appears due to loss of contraction of the ciliary muscle, loss of elasticity of the crystalline lens, reduction of elasticity in Bruch’s membrane, sclerosis with the age as due to changes in the diameter and thickness of the crystalline lens mainly. Because the changes that induce presbyopia with the age; it is necessary to plan treatment to restore the vision at near, intermediate and far distances. Furthermore, to ophthalmic lenses (New vision glasses), various ophthalmologic treatments have been developed to improve the vision in presbyopic patients. Concretely, scleral surgery, multifocal corneal excimer ablation techniques, monovision, intrastromal corneal devices or Premium Intraocular Lenses (IOLs) among others techniques have been introduced. For example, Premium IOLs are a recommendable alternative to restore the vision in patients older than 50 years of age at all distances due to provide good visual outcomes and minimal postoperative complications.
Different technologies for improving vision in presbyopic patients by means of intraocular lenses have been developed as refractive, diffractive, trifocal, extended depth-of-focus, hybrid refractive-diffractive, asymmetrical rotation or Accommodative IOLs. However, despite all the intraocular lenses provide good visual outcomes the only alternative able to physiologically restore the accommodation are Accommodative IOLs, which technology has advanced considerably.
What advances have been developed in Accommodative IOLs?
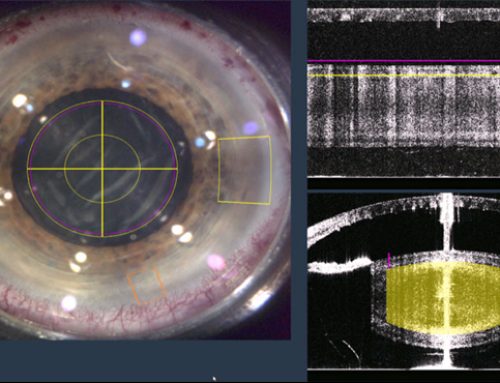
Since years ago, Accommodative IOLs have been investigated to restore the accommodation and improve the vision of presbyopic patients. During these years of research and clinical experience different Accommodative IOLs have been developed. Concretely, stand out the single-optic IOLs, dual-optic IOLs or those intraocular lenses that provide accommodation modifying its curvature or through fluids mainly. Furthermore, of the development of the technology the Accommodative Intraocular Lenses is very important to know its outcomes and its optical quality. Precisely, after cataract surgery is necessary to perform diverse diagnostic test to know the adequate position of the Accommodative Intraocular Lens inside the eyeball, its visual quality, its functionality and its accommodative ability mainly. For example, is important to know the outcomes of Accommodative IOLs to perform contrast sensitivity, defocus curve, ocular aberrations, visual acuity, reading speed, optical quality among others…
Likewise, important international scientific investigations about the technology and optical quality of the Accommodative Intraocular Lenses have been published in Pubmed Central database. For example, the Director of the course, Professor Jorge Alió has published recently in American Journal of Ophthalmology an investigation about the accommodation ability of a new intraocular laser AkkoLens Lumina compared with a standard monofocal IOLs. In the study, Alió et al included 61 eyes implanted with AkkoLens Lumina IOL, whilst 25 eyes were implanted with an Acrysof SA60AT monofocal IOL. Concretely, after 12 months of follow authors proved that Lumina Accommodative IOL restores the visual function, contrast sensitivity, and accommodation after cataract surgery. Because the high clinical, teaching and research experience of our international tutors, from the Online Course in Refractive Clinical Methodology Cataract and Corneal Surgery, provide widely information about the optical performance, technology, design and outcomes of different Accommodative Intraocular Lenses.
Scientific reference
Alio JL, Simonov A, Plaza-Puche AB, Angelov A, Angelov Y, van Lawick W et al. Visual Outcomes and Accommodative Response of the Lumina Accommodative Intraocular Lens. Am J Ophthalmol. 2016 Apr;164:37-48.