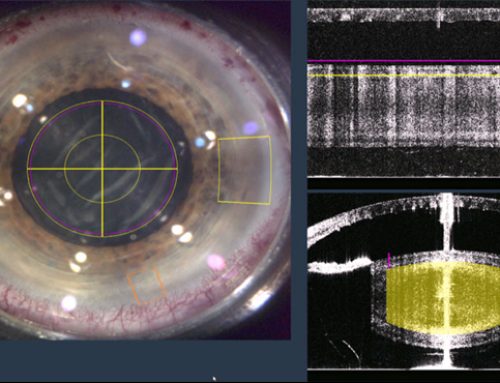
Cataract surgery is one of the most common surgical interventions worldwide to restore vision with a high success rate and patient cataract surgery satisfaction. In spite of the improvements made on this procedure, cataract surgery is not fully exempt from risks. Precisely, recent advances with the introduction of minimal incision cataract surgery (MICS), or the advent of femtosecond laser assisted cataract surgery (FLACS) have helped to reduce intra- and postoperative complications. Nevertheless, one of the most frequent evolutive “complications” that may occur months after the intervention of cataract or clear lens extraction is the Posterior Capsular Opacification (PCO). Precisely, the posterior capsular opacification occurs as a consequence of the fibrosis and opacification of the posterior capsule due to the migration of the lens epithelial cells that remain in the capsular bag after the intervention. Although posterior capsular opacification initially begins in the periphery, if it progresses can affect the central vision inducing a decrease in the visual acuity, alteration in contrast sensitivity and glare.
When it affects the central vision, it will be necessary to perform a Nd:YAG laser capsulotomy to restore the transparency of the lens and the vision. Precisely, in a scientific study published by Dr. Jorge L. Alió Del Barrio and colleagues in Archives of the Spanish Society of Ophthalmology proved that Nd:YAG capsulotomy is a safe procedure in pseudophakic patients without any other ocular pathology, improving the Best Corrected Visual Acuity (BCVA). However, in spite of being posterior capsular opacification a common complication after the substitution of the crystalline lens by an intraocular lens (IOLs), different improvements on its design and in the surgical procedure have been proposed to reduce its incidence.
What progresses have been developed to avoid posterior capsular opacification?
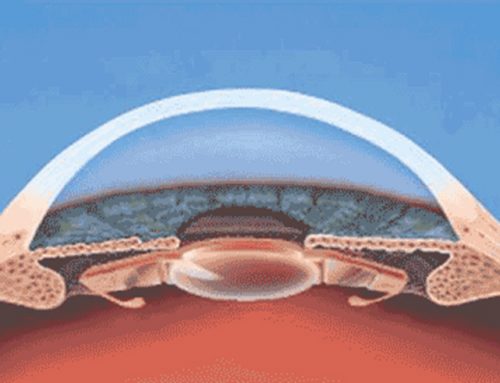
It is widely known that the advances developed in the technology of intraocular lenses have allowed improving vision at all distances, and evening in night conditions. Furthermore, intraocular lenses have incorporated improvements on their design and material that permits to reduce the incidence of posterior capsular opacification after cataract surgery or clear lens surgery. Precisely, the edges of the haptics of the intraocular lenses are designed with a special geometry that inhibits the proliferation of the epithelial cells. Concretely, intraocular lenses with a square edge design reduce considerably the incidence of PCO.
Besides of the design of the optic and haptics of the IOLs, there are other factors that allow reducing the incidence of PCO: a good capsular polishing at the end of the surgery, a capsulorhexis diameter lower than the IOL optical zone and the reduction of the irrigation-aspiration time. Moreover, viscoelastic with small concentration of hyaluronic acid prevents posterior capsular opacification. It is also suitable the use of capsular tension rings, especially in myopic patients.
In the Online Course in Refractive Clinical Methodology Cataract and Corneal Surgery we provide updated education about the design of intraocular lenses for the prevention of posterior capsular opacification.
Scientific reference
Ruiz-Casas D, Barrancos C, Alio JL 2nd, Ruiz-Guerrero M, Muñoz-Negrete FJ. Effect of posterior neodymium:YAG capsulotomy. Safety evaluation of macular foveal thickness, intraocular pressure and endothelial cell loss in pseudophakic patients with posterior capsule opacification. Arch Soc Esp Oftalmol. 2013 Nov;88(11):415-22.